For those who aren't familiar, before we talk about treatment, let's go over some basics about the kidneys.
What Do My Kidneys Do and What is Chronic Kidney Disease (CKD)?

Your kidneys filter your blood to remove waste and excess fluid which are then eliminated in your urine. If your kidneys aren’t working properly, waste products and fluid can build up and cause problems. The kidneys also make a hormone to stimulate the bone marrow to make red blood cells as well as convert the inactive form of Vitamin D to the active form which is necessary for calcium absorption from the diet and bone metabolism.
CKD is the progressive damage and loss of kidney function. Depending on many factors, it may progress slowly, or it may progress more rapidly. If the kidneys fail completely, you need dialysis to do the work of the kidneys.
Luckily, there are ways to slow down the progression of chronic kidney disease. Depending on the degree of damage, with comprehensive care, you may be able to live a normal life.
How Did I Get CKD and What are the Symptoms?
By far, the most common causes of CKD are diabetes and hypertension. Diabetes accounts for about 40% of all CKD, and hypertension accounts for about 35% of CKD. Other causes include autoimmune diseases such as glomerulonephritis and lupus, IgA Nephropathy, Polycystic Kidney Disease, chronic kidney infections, Hepatitis B and Hepatitis C, and certain medications and herbal products. 1 in 7 people in the U.S. have CKD, and many don’t know that they have it.
Physical symptoms don’t occur until kidney damage is advanced. Symptoms include fatigue, weakness, muscle cramps, generalized itching, fluid retention with swelling in your legs, feet, hands, and face, anemia, CKD bone disease that can cause bone pain, sleepiness, worsening hypertension, decreased appetite, neuropathy, cognitive impairment (decreased mental sharpness), sleeping problems, and elevated potassium levels that can cause abnormal heart rhythms.
Many of the above symptoms are not specific to kidney disease, and they can be due to other disorders, so be sure to see your health care provider to get the right diagnosis.
CKD doesn’t travel alone. It increases death from all causes, and especially from cardiovascular disease and an increased risk of cancer. The risk of death rises exponentially as kidney function declines. People with CKD are 5-10 times more likely to die of another cause than they are to live long enough to need dialysis.
If I Don’t Have Any Symptoms, How is it Diagnosed and Followed?
CKD is diagnosed and followed by blood tests including BUN (blood urea nitrogen), creatinine, and glomerular filtration rate or GFR for short. (The glomerulus is the unit that makes up the kidneys.) The lower the number, the more advanced the disease is.
CKD is also diagnosed and followed by looking at protein in the urine (usually albumin) and comparing it to the amount of creatinine in the urine known as urine albumin creatinine ratio (UACR). An elevated UACR can be an earlier sign of kidney damage than an elevated creatinine or a reduced GFR. People with protein in their urine are also at higher risk of CKD progression.
These blood and urine tests are basic tests commonly done on people with diabetes, hypertension, older age, heart problems, or routinely with an annual exam. By seeing your doctor regularly, CKD can be found earlier, and treatment can be started.
Treatments to Slow CKD Progression
Angiotensin Converting Enzyme Inhibitors (ACE Inhibitors) & Angiotensin Receptor Blockers (ARBs)
 These 2 classes of medicines work on the renin-angiotensin pathway, but at different sites in the process. The pathway is a major site for blood pressure control.
These 2 classes of medicines work on the renin-angiotensin pathway, but at different sites in the process. The pathway is a major site for blood pressure control.
ACE inhibitors and ARBs protect the kidneys and the cardiovascular system by reducing systemic blood pressure and the pressure within the glomerulus (basic unit of the kidney). This improves blood flow within the kidney and decreases protein from leaking into the urine (proteinuria).
Both ACE and ARBs decrease the risk of kidney failure and cardiovascular events.
ACE inhibitors are superior to ARBs for prevention of kidney events, cardiovascular outcomes, cardiovascular death, and all-cause mortality in non-dialysis patients with stage 3-5 CKD. However, some people can’t tolerate them due to cough, elevated potassium, and low blood pressure.
Angiotensin converting enzyme inhibitors (ACE Inhibitors) include medications such as: ramipril, lisinopril, benazepril, enalapril, quinapril and others ending in “pril”.
Angiotensin Receptor Blockers (ARBs) include medications such as Losartan, Valsartan, Olmesartan, irbesartan, and others ending in “sartan”.
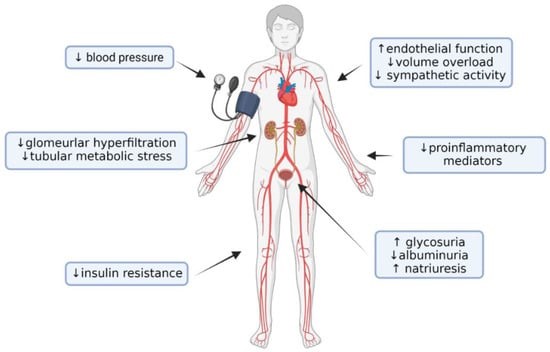
SGLT-2 Inhibitors (An Exciting Breakthrough in Treating CKD)
SGLT-2 inhibitors stand for sodium glucose co-transporter 2 inhibitors. They were first approved for the treatment of diabetes, but they are now shown to have benefits in CKD, cardiovascular disease, and congestive heart failure.
How Do They Work?
Normally sugar in the blood stream is filtered by the kidneys and is then reabsorbed by the kidney back into the blood stream. Inhibiting the SGLT-2 molecule blocks reabsorption of the sugar allowing it to be lost in the urine. This lowers blood sugar. Loss of sugar from the body can contribute to weight loss, and SGLT-2s also have a very mild effect on decreasing blood pressure.
What Are the Other Benefits Besides Treating Diabetes?
Dapagliflozin (Farxiga) was approved by the FDA to reduce CKD progression in diabetics and non-diabetics. Canagliflozin (Invokana) has also been approved to decrease CKD progression, but only in diabetic patients with existing CKD and albuminuria. Other SGLT-2s are also likely to decrease the progression of CKD, but official FDA approvals are pending.
Several SGLT-2s are approved to reduce cardiovascular death in diabetics with cardiovascular disease. This is very exciting given the markedly increased risk of cardiovascular disease in patients with CKD.
Several SGLT-2s have also been approved to reduce congestive heart failure in patients with or without diabetes.
Chase Medical Research has been and is currently involved in these pivotal trials regarding preventing progression of CKD and prevention of adverse outcomes in cardiovascular disease and congestive heart failure.
Beneficial systemic effects of SGLT2i with an impact on protection from CKD progression. Created with BioRender.com.
Non-Steroidal Mineralocorticoid Inhibitors
There are 3 drugs in this class: Finerenone (Kerendia), spironolactone, and Eplenerone (Inspra).
Finerenone is a 3rd generation drug, and is used for decreasing the progression of CKD because:
- It causes fewer problems with hyperkalemia (elevated blood potassium) than spironolactone and eplenerone.
- It is more selective for the mineralocorticoid receptors and has a stronger affinity for the mineralocorticoid receptors (binds more tightly) than Eplenerone.
- There is overactivation of the mineralocorticoid receptor in CKD and cardiovascular disease leading to inflammation and fibrosis (scarring). By inhibiting the mineralocorticoid receptor, Finerenone decreases inflammation and fibrosis, and it also decreases the UACR (Urine albumin to creatinine ratio) which is both a marker and symptom of CKD.
- Finerenone has also been shown to reduce cardiovascular death, non-fatal myocardial infarction, and hospitalization for heart failure in adult patients with CKD associated with diabetes.
GLP-1 Agonists (Glucagon Like Peptide-1 Agonists)
Like SGLT-2 Inhibitors, GLP-1 Receptor Agonists are diabetic drugs that have beneficial effects on CKD and the cardiovascular system.
There are GLP-1 receptors in the pancreas, lungs, brain, heart, and in the kidneys.
GLP-1's decrease UACR and slow the decline in the glomerular filtration rate (GFR). The benefits are not just due to the effects on decreasing blood sugar in diabetics.
Reducing intra-glomerular pressure, oxidative stress, resorption of sodium and subsequent diuresis, and reducing inflammation are proposed mechanisms in which GLP-1’s protect the kidneys and the cardiovascular system.
Indirect mechanisms by which GLP-1’s may help protect the kidneys include improving diabetic control, abnormal lipids, obesity, and hypertension.
Control of Diabetes, Hyertension, and High Cholesterol
Multiple studies have shown that good control of diabetes, hypertension, and cholesterol will slow the progression of CKD as well as other diabetic complications such as cardiovascular disease, neuropathy, and retinopathy (diabetic eye disease).
Diet
- Limit the salt and protein in your diet.
- Limit high potassium foods like potatoes, tomatoes, and citrus fruits.
- Stay hydrated. However, in very advanced CKD, your doctor may recommend that you limit your fluid, so make sure you check with your doctor before making any changes.
Lifestyle
- Maintain a healthy weight.
- Exercise
- Don’t smoke.
- Use caution regarding the use of herbal products and over-the-counter medications. Discuss their use with your health care provider before starting them.
There are pros and cons of all medicines, and not all medicines are right for everyone. Please discuss what choice is right for you with your health care provider.
Clinical Research
Chase Medical Research (CMR) is a leading research center and has conducted studies on the major medications that are now approved by the FDA and used in the treatment of CKD. CMR also does research trials on many other diseases such as diabetes, obesity, and cardiovascular disease. If you are interested in participating or just want to learn more about our trials, please check out our currently enrolling trials here.
References:
- Andrew Bental, MD; https://www.mayoclinic.org/diseases-conditions/chronic-kidney-disease/symptoms-causes/syc-20354521
- Bakris, George L., et al. “Effect of Finerenone on Chronic Kidney Disease Outcomes in Type 2 Diabetes: Nejm.” New England Journal of Medicine, 3 Dec. 2020.
- “Chronic Kidney Disease (Ckd).” National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd.
- “Chronic Kidney Disease.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 3 Sept. 2021, https://www.mayoclinic.org/diseases-conditions/chronic-kidney-disease/symptoms-causes/syc-20354521.
- Empagliflozin in Patients with Chronic Kidney Disease, The Empa Kidney Collaborative Group, January 12, 2023, N Engl J Med 2023; 388:117-127.
- “Facts about Chronic Kidney Disease.” National Kidney Foundation, 25 Feb. 2021, https://www.kidney.org/atoz/content/about-chronic-kidney-disease.
- KJ Mayne, SYA Ng, D Preiss, AJ Roddick, et al, Impact of diabetes on the effects of sodium glucose co-transporter-2 inhibitors on kidney outcomes: collaborative meta-analysis of large placebo-controlled trials. The Lancet, 11-2022; 400: 1788-1801.
- Posesta MR, Sabiu G, et. al. SGLT2 Inhibitors in Diabetic and Non-Diabetic Chronic Kidney Disease, Biomedicines Dec 20, 2023. Biomedicines 2023, 11(2), 279; https://doi.org/10.3390/biomedicines11020279.
- Webster, AC, Nagler EV, et. al, Seminar: Chronic Kidney Disease, published November 22, 2016, Lancet 389:10075; 1238-1252.
- Yaru Zhang, #1 Dandan He, et al. ACE Inhibitor Benefit to Kidney and Cardiovascular Outcomes for Patients with Non-Dialysis Chronic Kidney Disease Stages 3–5: A Network Meta-Analysis of Randomised Clinical Trials; National Library of Medicine, Drugs. 2020; 80(8): 797–811. Published online 2020 Apr 24. doi: 10.1007/s40265-020-01290-3.
- Yu JH, Park SY et al., GLP-1 Receptor Agonists in Diabetic Kidney Disease:current evidence and future directions, Kidney Res Clin Pract. 2022 Mar; 41(2): 136–149.
Share This Post
Recent Posts
- The Relationship Between Obesity and Obstructive Sleep Apnea March 28 2023
- Cardiovascular Outcome Clinical Trials March 28 2023
- Diabetic Peripheral Neuropathic Pain March 28 2023
- Are All Types of Cholesterol Bad? March 28 2023
- Blood Pressure: The Highs, the Lows, and Everything in Between March 28 2023
Categories
- Clinical Trials
- Cardiovascular Disease
- Diabetes
- Obesity
- Kidney Disease
- Hypertension
- Pain Management
- Vaccine
- Cholesterol
- Chronic Obstructive Pulmonary Disease
- Diabetic Peripheral Neuropathy
- Migraine
- Osteoarthritis
- Biologics
- COVID-19
- Gastroesophageal Reflux Disease
- Irritable Bowel Syndrome with Constipation
- Lyme Disease
- Nonalcoholic Steatohepatitis
- Respiratory Syncytial Virus